Colorectal cancer – common diagnosis
Colorectal cancer of the colon and rectum is one of the most common cancer diagnoses in Germany. Due to good treatment options, the survival rate is relatively good (surveys by the Robert Koch Institute). Treatment by chemotherapy or surgery is often combined with adjuvant radiation therapy in the rectal area for successful treatment.
1 from 8
of new cancer cases are in the colon or rectum
approx. 66 %
of malignant tumors are colon tumors
Ø approx. 65 %
relative survival rate after five years
Source: “Cancer in Germany”, RKI/Krebsdaten.de
Where can you have colorectal cancer treated in Munich?
The treatment of patients with bowel cancer can be carried out with the help of various procedures. The team of Radiologie München supports colleagues from other disciplines in tumour boards to develop an individual treatment plan for rectal or colorectal carcinomas according to the patient’s state of health in order to ensure the best possible therapy.
What is a tumor board?
Tumour boards are conferences in which specialists from different fields discuss the respective case together. In doing so, they jointly determine the optimal strategies for diagnostics and therapy.

Colorectal cancer – how does treatment begin?
If a patient is diagnosed with colorectal cancer, it is usually a tumour in the large intestine (colon carcinoma) or in the rectum (rectal carcinoma). Depending on the general condition and stage of the disease, the doctors at Radiologie München work out a treatment plan together with the patient and the colleagues in oncology or surgery to treat the cancer.
How is colorectal cancer treated?
Decisive for the efficient treatment of colon or rectal cancer is the position of the cancer in the colon, its stage (T I-IV) or classification (UICC I-IV), and its spread. The patient’s risk of relapse and overall health are also considered. Depending on the diagnosis, surgery, chemotherapy, radiation therapy or targeted therapies may be considered for treatment.
Radiotherapy
Neoadjuvant (= preoperative) radiation is mainly used for rectal tumours; it plays a rather minor role in the treatment of colorectal cancer. At a very advanced stage, radiotherapy is useful for both cancers if metastases have been diagnosed in the bones or brain.
Radiation therapy is intended to slow down the spread of the malignant cells, alleviate symptoms and thus improve the patient’s quality of life. In percutaneous radiation (teletherapy), which is performed on an outpatient basis, tumor cells are destroyed with high-energy radiation from different directions.
The radiation fields include the cancer and the affected surrounding tissue. The treatment plan ensures that the high-energy radiation only irradiates the malignant cells and not the healthy tissue.
Operation
Small, superficial tumors may be removed endoscopically. Larger tumors must be surgically removed. The extent of this surgery depends on whether the cancer is localized or whether surrounding tissues or lymph nodes are also affected. Depending on this, different parts of the intestine, surrounding tissue or the lymph nodes may also need to be removed.
In the case of a tumor in the rectum, it may also be necessary to create an artificial bowel outlet(stoma or anus praeter). Neoadjuvant chemotherapy or radiation therapy or their combination (radiochemotherapy) may also be used before surgery if the cancer is advanced, deep-seated, or has spread to surrounding tissue.
The goal here is to shrink the tumor enough to allow surgery or to reduce the extent of surgery. Whether it is used also depends on how high the treating doctor assesses the risk of relapse
Chemotherapy
Chemotherapy may be useful in advanced stages of cancer in addition to neoadjuvant use after surgery. The aim of this adjuvant (= supportive) chemotherapy is to reduce the risk of relapse. The treatment acts systemically throughout the body and can damage scattered cancer cells. Chemotherapy may also be the treatment of choice when the cancer or metastases are inoperable. In this case, coordinated chemotherapy and targeted drugs are used in an attempt to reduce or stop tumor growth.
Targeted drugs
Modern cancer-specific drugs are mainly used in advanced colorectal cancer. Most often, these are prescribed in addition to chemotherapy. These drugs additionally stop cell growth and thus stop the spread in the body.
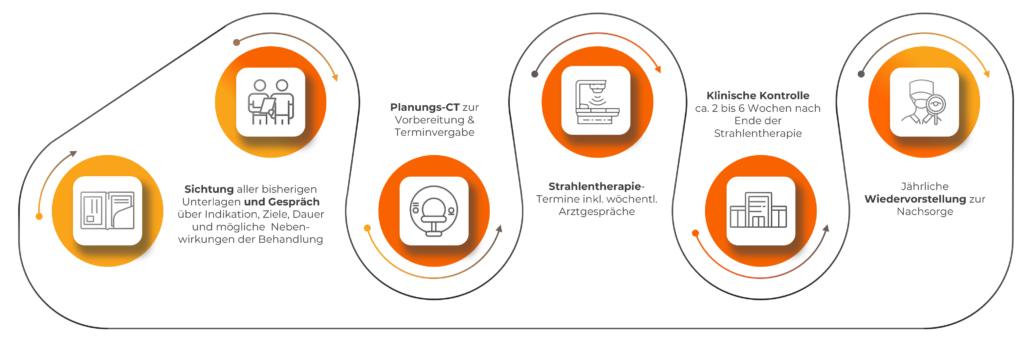
What is the treatment process in our practices?
What do you need to pay attention to before, during and after treatment?
Please discuss possible treatment options and consequences with your treating physician. Patients with an artificial bowel outlet in particular have to get used to a change and often feel that their quality of life is restricted. He or she will be happy to provide you with information about possible support options or rehab and follow-up care.
Please make sure you eat a healthy, balanced diet and drink enough water. A healthy nutritional status plays an important role in the treatment and spread of the tumor. It also helps reduce the side effects of therapy. Alcohol and smoking are largely prohibited.
What are the side effects of colorectal cancer treatment?
The therapy is individually tailored to the patient so that it fights the cancer as efficiently as possible. However, side effects may still occur during or after treatment.
Depending on the extent of the surgery, the procedure and its consequences can be stressful for the patient: complications, infections, nerve damage, bowel obstructions, incontinence, lymphedema or effects on the bladder may occur.
Cytostatic drugs used in chemotherapy and radiation therapy affect the hematopoietic cells of the bone marrow, weakening the immune defenses and causing the patient to feel debilitated. Nausea, diarrhea, inflammation of the mucous membranes, skin problems and hair loss are also frequently observed. Tissue around the bowel, bladder or genital tract may be affected.